How HVAC Airflow Affects the Spread of Coronavirus (COVID-19)
In order to reduce the possibility of COVID-19 spreading in its waiting and treatment areas, the Vatican State Children’s Hospital took many precautions. Facilities managers needed to decide whether to turn on the air conditioning as the summer heat wave approached.
Which made closed rooms with increased airflow safer for patients: less or more? Ansys Fluent was utilized by computational fluid dynamics (CFD) experts at Ergon Research in Florence to provide answers to these queries.

Employing CFD (Computational Fluid Dynamics) to Analyze In-Building Transmission of COVID-19
The new coronavirus struck Italy quickly and severely. A scary statistic at the moment, the nation was reporting an average of more than 6,000 new cases each day by the end of March 2020. That month, a statewide lockdown was instituted, which was successful in lowering the number of daily new cases.
To provide more background to the study, at this time, most of Italian life did not return to normal until May, when eateries, bars, and other gathering places were allowed to reopen (though with strict social distancing protocols in place).
It’s one thing to live under lockdown during an Italian spring. Both the heat and the air conditioning could be turned off and one could still live comfortably. Italian hospitals were highly concerned about the possibility of a secondary health crisis brought on by residing or working in enclosed quarters without air conditioning.
CFD Research Provides Italy with Insights to Mitigate Risk of COVID-19 Spread in Hospitals
The OPBG, a prestigious pediatric hospital run by the Vatican, faced a significant operational dilemma for its management in the wake of this problem. Would the risk of virus transmission to people who are otherwise healthy increase or decrease if the heating, ventilation, and air conditioning (HVAC) system was activated in a hospital waiting room or treatment area?
More questions arose. Would uninfected people in that room be safer if the air was moving or still if an unmasked person with COVID-19 coughed or sneezed, even if they were seated at a suitable social distance from someone else? Droplets of a virus may have been prevented from spreading and infecting others by still air. However, flowing air might assist the droplets leave the room faster by diffusing viral concentrations more quickly.
A hospital employee named Dr. Luca Borro started posing inquiries in a Facebook group in April 2020 about utilizing CFD to model a cough or sneeze event and simulating what would occur with the HVAC system running. Borro is a specialist in 2D and 3D imaging, but he needed assistance with some CFD modeling-specific problems despite this.
His unexpected encounter with Lorenzo Mazzei, a team member from Ergon Research, sparked a partnership in which CFD specialists from Ergon Research contributed their time and knowledge to assist the hospital in obtaining preliminary answers to these issues.
Creating A New CFD Model: Overcoming Design Challenges to Simulate Airflow
The research, employing Ansys Fluent software, was used in the CFD experiments to simulate the airflow due to precision and rapid computational abilities.
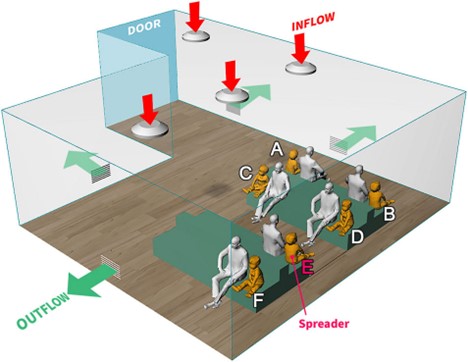
Two CAD models of a waiting area and a treatment room were first built by the team. The waiting room model had several sitting characters as well as benches for chairs. The model contains an equal number of adult and kid figures because the Vatican State Children’s Institution is a pediatric hospital.
Along with pairing up the adults and kids, the model placed the pairs at the advised 6-foot distance from one another rather than the individuals, as one might anticipate seeing parents and kids doing in a pediatric waiting room. When the HVAC system was running, the waiting room model’s four ceiling-mounted air diffusers would produce a controlled positive airflow into the space.
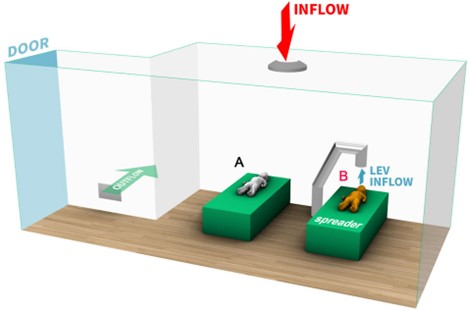
Four wall vents that would remove the air from the room were also taken into account. The treatment room model had a single ceiling diffuser, a single exhaust grate on the wall, and a local exhaust ventilation (LEV) system that was designed to draw air into a vent that was located immediately over the patient’s bed.
These CAD models were purposefully kept simplistic in several aspects. The generic, circular ceiling air diffusers, for instance, solved the interior flow field rather than imposing it on the boundaries by included the deflectors in the simulation.
Since the introduction of elements like chair arms, legs, and backs would not have significantly changed the informational outcome of the simulations Ergon had planned, no features were present on the furniture. Additionally, they would have significantly increased the amount of processing time and resources needed to execute the simulations. For the same reason, the physical characteristics of the people and kids in the room were also simplified, while being more detailed than the furniture.
Validating CFD Analysis with Eulerian-Lagrangian Simulations
The researchers at Ergon Research added these event features, droplet characteristics, the interaction of the aerosolized droplets with air molecules, and the buoyancy effects on both liquid particles and air due to gravity into Fluent using their knowledge with CFD simulations.
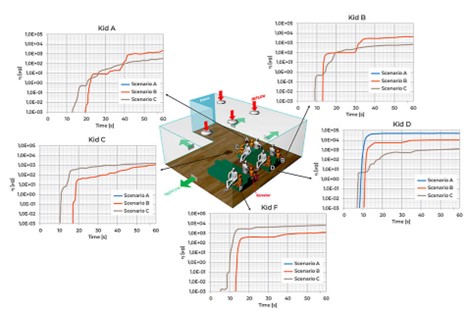
They also included models for the mass percentage of coughed air inhaled as well as models for the rates of respiration and inhalation for each person in the room (that is, the portion of contaminated particles contained in any inhalation after the cough event itself).
In order to study the dispersion and possibility for inhalation of aerosolized cough droplets inside each of the room models they had constructed, coupled Eulerian-Lagrangian simulations were undertaken.
Embedded Particle Injection and Tracking within CFD Simulations
There was no need to implement missing models because several essential modeling elements, like particle injection and tracking, were already included in Fluent.
Furthermore, Fluent had already undergone validation and verification against thousands of studies looking at Eulerian-Lagrangian simulations. The team simplified the CAD models of the rooms to meshes of just 5M elements.
This would save compute resources and time without sacrificing the clarity of the results Ergon Research was after. Additionally, the engineers wanted to use an event time step of 0.001 seconds and monitor the movement of the aerosolized particles for an entire 60 seconds.
CFD Simulation Scenarios of Waiting Rooms during COVID-19 Outbreak
They next employed the waiting room model to run a number of simulation scenarios, including:
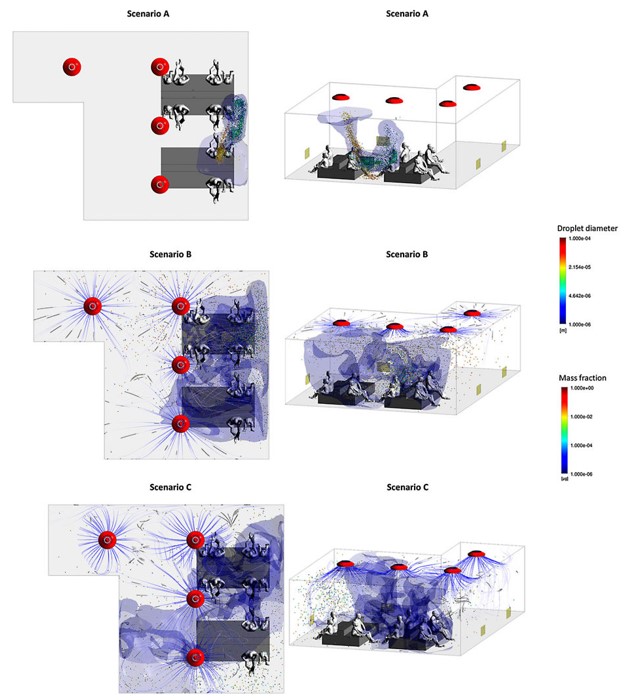
- Simulation A was completed without the use of HVAC-mediated airflow.
- Simulation B includes 2020 m3/hr of airflow through the diffusers (the standard flow rate)
- Airflow in Simulation C was at a 4040 m3/hr flow rate, which is twice the typical flow rate.
Similar simulations using the LEV system in the treatment rooms (with the LEV inlet vent placed above the spreader patient’s mouth and calibrated to exhaust air from the room) were performed on the model by the fluids engineers.
With a pressure-based solver, a semi-implicit method for pressure-linked equations (SIMPLE) algorithm, a second-order upwind scheme for all variables (aside from turbulence quantities), and a bounded second-order implicit scheme for time, the solutions were achieved.
Critical CFD Research Enable a Practical Hospital Treatment Plan during COVID-19
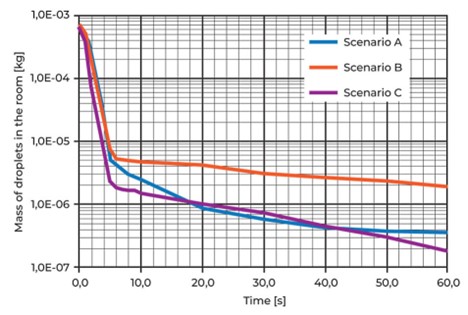
The initial findings from the simulations in Fluent were reliable, consistent, and somewhat unexpected. Regardless of HVAC flow rate, in all waiting room simulations, aerosolized droplets bigger than 100 m tended to gravitate toward the ground whereas smaller, lighter droplets distributed across the space in a variety of conditions:
- When there was no HVAC-mediated airflow in scenario A, the lighter droplets traveled straight toward the individual seated across from the cougher (the spreader). Only the person standing across from the spreader appeared to breathe in any appreciable amount (11%) of contaminated air.
- In simulation B, which uses the typical HVAC flow rate of 2020 m3/hr, the lighter cough droplets interact with the diffuser airflow before they concentrate on the child seated in front of the spreader and are quickly disseminated across the space. As a result, fewer contaminated droplets are breathed by the person seated across from the spreader than they may have been had there been no airflow in the space (from 11 percent down to 2.5 percent ).
- Additionally, it spreads contaminated droplets about the room more extensively and offers a tiny chance for people to inhale such droplets. The air that people closest to the spreader might breathe contains 0.5 percent polluted droplets.
- When the HVAC flow rate is increased to 4040 m3/hr in simulation C, the aerosol cloud is completely disrupted and quickly dispersed throughout the space. While this does expose people in the entire area to contaminated droplets, the greater turbulence also accelerates the rate at which the wall vents remove the droplets from the space by dilating the concentration of contaminated droplets (at which point they no longer pose a risk to the individuals in the room).
- Those seated closest to the spreader are only breathing in air with a 0.3 percent concentration of infected droplets 30 seconds after the coughing episode, while those seated farthest from the spreader are only breathing in air with a 0.08 percent concentration of contaminated droplets.
- The results from the treatment room simulations were even more striking: when the LEV, which was placed just above the patient’s head, was activated to draw air away from the patient at a rate of 1080 m3/hr, all infected droplets were drawn out of the room within half a second of the spreader coughing, greatly reducing the chance that anyone else in the room would catch an infection from the droplets in the cough.
Conclusion | Ansys Fluent Simulations Aid Hospital Administrators during COVID-19
The Vatican State Children’s Hospital received the findings from Ergon Research’s simulations as the heat of Rome’s summer approached.
The results of the simulations performed in Fluent indicated not only that the HVAC system in the hospital waiting rooms be turned on, but also that the airflow rate be increased. When the flow rate is increased, air turbulence in the space can decrease the amount of contaminated particles by 99.6% in a matter of seconds, lowering the risk that other patients would contract the infection via a cough.
Similar to this, using an LEV system in a treatment room could immediately reduce exposure risk. The struggle against COVID-19 would still be difficult for hospital administrators and medical staff. However, doctors wouldn’t have to be concerned about making matters worse by seeing an increase in patients who were experiencing heatstroke while seated in warm rooms.